We were becoming more and more alarmed as we realized Anna was not getting better. We were already doing therapy (nebulizer & chest percussion for 20 min) three times a day at home. (I say "we" but it is really Wende who is the hero in this story. I get to leave the house and hang out in the world of grown-ups all day at work. She is the one taking care of EVERYTHING-- using her supernatural gift to organize, educate and provide a sense of order and foundation amid the chaos of our infant and the other 4 children whom I affectionately refer to as Madame Curie and the Three Stooges. While Padre Pio may have had the supernatural gift of bilocation, Wende has the gift of being organized, and as St. Josemaria Escriva said "being organized multiplies your time." But I digress...) Anna had been on three different rounds of oral antibiotics for the last 6 weeks. Was this "just the CF" symptoms starting to show up or was this an infection? If it was viral, why was it being aggressively treated with antibiotics? Why wasn't she getting better? Dr Akhter informed us that he would like to have her hospitalized, put on IV antibiotics and receive more intensive treatment. Wende and I initially said no and wanted to give it another week. We were caught off guard, not to mention that there are logistics involved concerning the other 4 kids.
We were told if Anna was not significantly better by the following Thursday she would be admitted into the hospital, so we should "have our bags packed" when we came follow-up visit. My feelings of alarm had turned into fear.
That next week was spooky. The blizzard hit, I stayed home from work for a few days. Anna's labored breathing continued and her chest and neck retractions were as plain as day. By the time Thursday rolled around they had finally plowed our street (it took 2 days after the snow stopped) and we could get out of our driveway. Wende and I were both mentally prepared to have her hospitalized. We had also arranged the logistics for the other kids. Getting Anna into the hospital ended up being an all-day event. When we arrived at Hope Children's Hospital to meet the CF team before she was to be admitted, we were told that they couldn't admit her. There were no beds available. Probably not that day. Maybe not even Friday. I couldn't believe we were being sent home. We went back to pick up the kids and waited at my mom's house for a few hours. I called the "bed coordinator" and pleaded with her if there was anything she could do to get us in. She informed me that there were 8 other children ahead of us waiting for a bed. It was late, so we drove home to Joliet, and as we were pulling in to the driveway, I received a call that they could put Anna in the ICU if we turned around and came in immediately. We turned around and finally got her in.
Anna was at Hope Children's Hospital for a week. Wende stayed with her and did not set foot out of the hospital that whole time. Our doctor showed us her chest xrays compared to her normal, baseline films taken just 1 month prior. I was shocked at how dramatically different the two films were. The radiologist who read her films called it pneumonia, and I suppose that is a way to describe what her symptoms. And evidently that is an academic debate and a matter of semantics as our pulmonologist said it is not "pneumonia," it is a "pulmonary exacerbation." "P.E. is the code-word now." ...got it.
So, to put the pieces of the puzzle together: the cold or virus that Anna had evidently caused her cystic fibrosis mucus-thickening-can't-get-it-out-of-you mechanism to kick-in high-gear. Dr Akhter told Wende that he had not seen such severe CF symptoms in someone so little. That was tough to hear. You never like to hear a specialist tell you news like that. CF treatment and management is supposed to be a long-term game plan, not a "4th quarter and the team is down 14 points" game plan.
Anna's therapy was upped to 4 times a day. She was put on Pulmozyme, which breaks down mucus and helps people with CF cough it out-- but most CF patients aren't on this medicine until later in life. She was on IV antibiotics even though her cultures did not show anything bacterial.
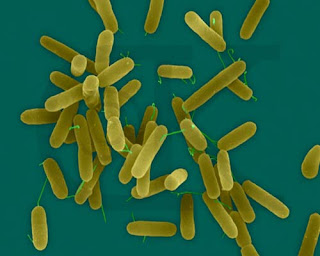
Worst case scenario would be that she came up positive for a type of Pseudomonas -- a bacterium that people with CF get-- the proverbial "CF Bug" that never leaves once they get it. God Be Praised they didn't find that.Over the week her oxygen saturation improved and her respiration rate became more normal. The chest retractions improved too. Except for the nurses who changed her IVs, Anna greeted everyone with a smile. This is not the Proud Pappa making overly sentimental platitudes-- she really smiled. On more than one occasion Wende was told by the staff that it was "nice to have a happy baby." I wish Anna had words. In her own little way she evidently brightened the day for a few others.
Anna was discharged from the hospital last Thursday and we see our CF team tomorrow. She'll have a follow-up chest xray in a couple weeks to see how her lungs are looking. Wende told me today that she could barely notice the chest retractions. Thank you everyone for your prayers. Please keep it up.
.